Introduction
Artificial intelligence (AI) in healthcare and medicine is rapidly transforming the way we prevent, diagnose, and treat illness. Over the next 10 to 50 years, advancements in AI will dramatically reshape medical practices, promising both profound benefits and significant ethical challenges.
Why AI Matters in Healthcare
AI’s potential to improve healthcare is enormous. Already, algorithms are helping doctors diagnose diseases earlier and with greater accuracy. Robotic technologies assist surgeons, while AI-driven data analysis personalizes treatments based on a patient’s unique genetic makeup. Consequently, these advancements can greatly enhance patient outcomes, streamline care delivery, and even extend human lifespan.
Addressing Ethical and Societal Impacts
However, the rise of AI also brings important ethical concerns. Data privacy, healthcare accessibility, patient autonomy, and algorithmic biases are critical issues demanding thoughtful attention. Without careful management, AI may inadvertently widen existing healthcare disparities, compromise patient trust, or lead to reliance on technology at the expense of human compassion.
Shaping a Positive Future
Therefore, actively addressing these concerns today is essential for realizing AI’s benefits tomorrow. In this article, we’ll explore key predictions about AI’s role in healthcare, highlighting opportunities and ethical pitfalls. Additionally, we’ll outline practical steps individuals and organizations can take to ensure AI supports a healthier and more equitable future.
AI in Diagnostics and Early Disease Detection
Transforming Medical Imaging with AI in Healthcare
AI in healthcare is already revolutionizing diagnostic capabilities. Currently, medical imaging techniques like X-rays, MRIs, and CT scans significantly benefit from AI-driven analysis. AI algorithms can quickly detect subtle anomalies—often faster and more accurately than human specialists. For instance, AI systems analyzing mammograms have increased breast cancer detection rates, potentially saving thousands of lives annually by identifying diseases at earlier, more treatable stages.
How AI Diagnostics Save Lives through Early Detection
Early disease detection greatly improves patient outcomes. With AI’s analytical strengths, healthcare providers can identify illnesses before symptoms even appear. Over the next decade, doctors will increasingly rely on AI-powered diagnostic tools integrated into routine care. Wearable technologies coupled with AI could continuously track vital signs and health indicators, signaling potential issues long before they become critical.
Ethical Challenges for AI Diagnostic Tools
Despite these advancements, significant risks remain. AI systems depend heavily on the quality and diversity of their training data. When datasets lack representation of minority groups, diagnostic errors become more likely, disproportionately affecting underserved populations. This risk makes equitable data collection critical.
Furthermore, patient trust is paramount. People want transparent explanations for AI-generated diagnoses, especially for serious conditions like cancer. To maintain patient trust, human oversight must remain central. Doctors using AI diagnostics need adequate training to understand algorithmic limitations, ensuring patient safety and confidence.
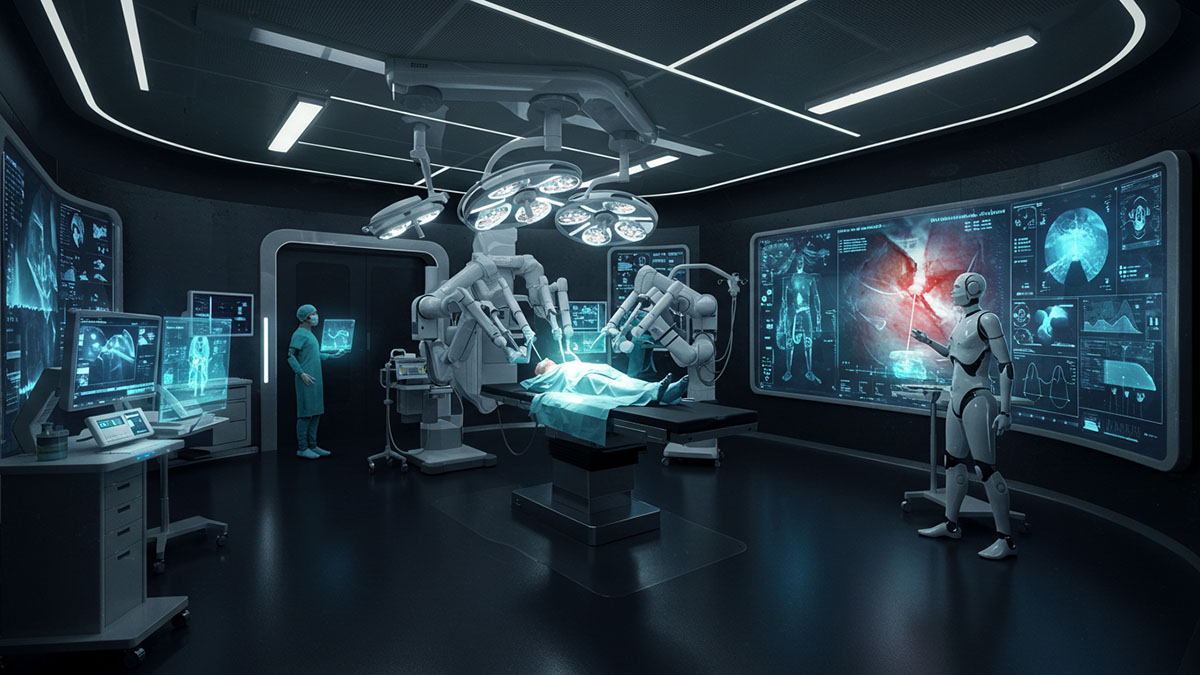
AI in Surgery and Patient Care
How AI in Healthcare Enhances Surgical Precision
AI in healthcare is significantly enhancing surgical capabilities. Today, robotic-assisted surgeries allow surgeons to perform complex procedures with greater accuracy and less invasiveness. AI-driven robotics provide real-time guidance, improving precision in delicate operations like heart surgery, joint replacements, and tumor removals. For instance, robotic systems guided by AI algorithms can precisely navigate around critical tissues, significantly reducing the risk of complications.
AI in Patient Care: Automating Routine Tasks
Over the next two decades, automation will expand beyond surgery into routine patient care. AI-powered systems could manage tasks such as medication administration, vital signs monitoring, and patient data collection. Virtual nursing assistants, equipped with AI, might monitor patient conditions continuously, alerting human staff to significant changes promptly. Consequently, hospitals could deliver safer, more efficient care, reducing staff burnout and operational costs.
Ethical Concerns with AI Healthcare Automation
Despite the clear benefits, expanding automation raises important ethical concerns. One critical issue is accountability: who is responsible if an AI-guided robot makes a mistake during surgery? Clear regulations and oversight structures must emerge to address liability and ensure patient safety. Additionally, human touch remains essential to healthcare. Automation should not reduce meaningful patient-provider interactions. Instead, AI should handle repetitive tasks, allowing clinicians to spend more time delivering compassionate, patient-centered care.
Personalized Medicine Powered by AI
AI in Personalized Healthcare: A New Era
AI-driven personalized medicine promises a future where treatments precisely match an individual’s genetic makeup, environment, and lifestyle. Today, doctors already use AI algorithms to analyze genetic information, helping select effective treatments, especially in oncology. Over the next decade, personalized therapies will likely become routine, significantly improving treatment outcomes and minimizing adverse reactions. For example, AI-powered genomic testing could predict how specific cancers respond to targeted therapies, substantially increasing survival rates.
Digital Twins and AI-driven Healthcare
Looking further ahead, AI could create virtual models known as “digital twins,” simulating a person’s unique biology. These advanced digital replicas could enable healthcare professionals to test treatments virtually before actual implementation. As a result, patients would receive optimized care plans tailored specifically to them. This approach might dramatically reduce treatment errors, ensuring safer and more effective healthcare.
Privacy and Ethical Issues in AI Personalized Medicine
However, personalized medicine relies heavily on sensitive data, including genetics and detailed personal health records. Therefore, robust data security and clear patient consent practices are essential. Patients need assurance that their private information is safe from misuse or unauthorized access. Furthermore, avoiding algorithmic bias is crucial. Ensuring data diversity is key, preventing the inadvertent exclusion of minority populations from the benefits of personalized medicine. If handled responsibly, AI-driven personalization could significantly enhance healthcare quality and patient trust.
AI in Longevity Research
Extending Human Lifespan with AI in Healthcare
Artificial intelligence is poised to revolutionize longevity research by significantly extending human life expectancy. Currently, researchers leverage AI to analyze massive datasets on genetics, metabolism, and aging biomarkers. These advanced AI models rapidly identify complex patterns associated with aging, revealing promising targets for intervention. As a result, within the next 10-25 years, healthcare providers may routinely recommend personalized anti-aging strategies based on AI-driven insights. This approach could slow the aging process, allowing people to remain healthier and active far longer than previous generations.
AI Predictive Tools for Healthy Aging
Additionally, predictive tools powered by AI could accurately assess biological age versus chronological age. These precise assessments enable doctors to suggest interventions tailored specifically to an individual’s unique aging trajectory. For instance, personalized lifestyle changes, targeted therapies, or supplements might effectively delay or even reverse age-related decline, significantly enhancing quality of life.
Ethical Impacts of AI-driven Longevity
However, extended longevity raises crucial ethical questions. Policymakers must address fairness, ensuring advancements in anti-aging technologies benefit all socioeconomic groups equally. Without careful oversight, longevity enhancements could exacerbate existing inequalities, providing lifespan advantages primarily to affluent populations. Moreover, extending life expectancy has implications for economic structures, retirement systems, and global resources. Proactive measures and thoughtful policies will be essential in balancing these advancements with social and ethical responsibilities.
AI in Drug Discovery and Biotechnology
AI in Healthcare: Accelerating Drug Development
AI is rapidly transforming drug discovery and biotechnology, significantly reducing the time and cost associated with bringing new treatments to market. Currently, traditional drug discovery processes are lengthy and expensive, often taking over a decade and billions of dollars. AI-driven platforms, however, streamline this process by rapidly identifying promising drug candidates, predicting efficacy, and minimizing risks early on. For example, recent AI-driven breakthroughs have shortened the discovery phase from several years to mere months, particularly in complex areas such as rare diseases and cancers.
AI-powered Biotechnology for Complex Diseases
In the next two decades, AI-powered drug discovery will likely revolutionize treatments for diseases currently deemed challenging or incurable. Conditions such as Alzheimer’s, autoimmune disorders, and rare genetic diseases stand to benefit significantly. By analyzing vast genomic and proteomic datasets, AI can identify novel targets and propose effective treatments previously overlooked by traditional research methods. As a result, patients could experience faster access to innovative and potentially life-saving therapies.
Managing Ethical Risks of AI Drug Discovery
Despite promising advancements, AI biotechnology also introduces potential ethical risks. AI-driven systems designed for beneficial medical purposes could inadvertently generate harmful compounds. Therefore, strict oversight and regulatory frameworks are crucial. Clear ethical standards, transparency, and robust safeguards will ensure AI in biotechnology remains a positive force, significantly benefiting human health without compromising safety or ethical integrity.
AI for Public Health and Preventive Medicine
AI in Healthcare: Revolutionizing Disease Prevention
AI’s integration into public health could dramatically enhance disease surveillance, prediction, and prevention. Currently, healthcare providers rely on limited data and manual analysis, often responding only after outbreaks occur. AI changes this dynamic by analyzing massive volumes of data—from environmental conditions and social media trends to clinical reports—to accurately predict potential disease outbreaks. Consequently, healthcare systems could respond proactively, minimizing impacts through early interventions and resource allocation.
Improving Health Equity through AI Public Health
Over the next decade, AI-powered public health tools have the potential to significantly improve healthcare accessibility worldwide, especially in underserved regions. For instance, AI applications could optimize vaccine distribution, predict chronic disease hotspots, and target public health campaigns more effectively. Moreover, smart public health infrastructure—such as AI-driven wastewater monitoring—could quickly identify disease surges in local communities, enabling rapid response and containment. This proactive approach could reduce global health disparities, bringing quality care to regions that previously lacked adequate resources.
Addressing Ethical Concerns in AI Public Health
However, utilizing AI for public health also raises important privacy concerns. Public health AI often depends on extensive personal data collection, posing potential privacy risks. Without robust safeguards and clear communication, these practices could undermine public trust. Additionally, algorithmic biases might inadvertently reinforce healthcare inequalities, prioritizing certain groups over others unfairly. Ensuring transparency, privacy protection, and fairness in AI systems will therefore be crucial in realizing the benefits of AI-powered preventive medicine.
AI in Mental Health Support
Expanding Access with AI Mental Health Support
AI-driven mental health technologies, such as chatbots and mobile apps, offer accessible support for millions facing mental health challenges. Currently, many individuals hesitate to seek help due to stigma, high costs, or limited availability of professional therapists. AI chatbots provide immediate, anonymous, and judgment-free assistance at any hour, using proven therapeutic techniques like Cognitive Behavioral Therapy (CBT). For instance, early evidence indicates chatbots such as Woebot can effectively reduce symptoms of anxiety and depression, offering meaningful support to those reluctant to seek traditional care.
Personalized Mental Health Care using AI
Within the next decade, AI tools will become increasingly sophisticated, delivering highly personalized mental health interventions. By analyzing subtle cues from users’ speech patterns, text inputs, or wearable sensor data, these advanced systems can detect emotional changes early, tailoring responses and therapeutic recommendations accordingly. Consequently, users might benefit from more proactive, continuous mental health support, significantly improving overall well-being.
Ethical Issues in AI Mental Healthcare
Yet, integrating AI into mental healthcare comes with notable ethical concerns. AI tools, regardless of sophistication, cannot fully replicate genuine human empathy or intuition. Misuse or overreliance on AI could lead to inappropriate care, potentially exacerbating serious mental health crises. Additionally, safeguarding user privacy is paramount, given the sensitivity of mental health data. Ensuring proper regulation, transparency, and human oversight will therefore be essential in effectively integrating AI into mental healthcare, reinforcing—not replacing—human-centered care.
Ethical and Societal Impacts of AI in Healthcare
Safeguarding Data Privacy in AI Healthcare
As AI becomes deeply embedded in healthcare, protecting patient privacy and data security will become increasingly crucial. Currently, AI systems rely on large datasets containing sensitive personal health information. Without robust privacy safeguards, there’s a real risk of data misuse or breaches, potentially eroding patient trust. Therefore, healthcare organizations must establish transparent practices, strong encryption, and clear consent protocols to ensure patient information remains secure. By prioritizing data protection, providers can confidently leverage AI while maintaining patient trust and safety.
Reducing Inequality through AI in Healthcare
AI has the potential to either bridge or widen healthcare gaps, depending on how thoughtfully it’s implemented. Ideally, AI-powered tools could significantly democratize healthcare, bringing advanced diagnostics and treatment recommendations to underserved communities. However, without careful planning, AI may exacerbate disparities by disproportionately benefiting wealthy regions or populations. To mitigate these risks, policymakers and healthcare providers must deliberately promote equitable AI adoption, ensuring underserved communities receive equal access to advanced AI healthcare solutions.
Preventing Bias in Healthcare AI Algorithms
Algorithmic bias remains a critical ethical concern. AI systems trained on incomplete or biased datasets can unintentionally amplify existing inequalities. For instance, algorithms trained predominantly on certain ethnic groups may perform poorly or inaccurately for others, compromising patient safety. To address this, diverse, representative datasets and routine algorithm audits should become standard practice. Ultimately, proactive measures and ongoing oversight will be essential to ensuring AI-driven healthcare solutions remain equitable and beneficial to all.
The Future of AI in U.S. Healthcare
AI in U.S. Healthcare: Tackling Costs and Outcomes
The United States faces unique healthcare challenges, combining advanced medical technologies with disproportionately high costs and relatively poor outcomes. Currently, despite spending more per capita than any other developed nation, the U.S. healthcare system struggles with inefficiencies, administrative burdens, and inconsistent patient care quality. AI presents an opportunity to address these challenges by streamlining administrative tasks, reducing wasteful spending, and enhancing overall efficiency. For example, AI-driven automation could simplify insurance billing, speed up claims processing, and lower overhead costs significantly.
Improving Coordination with Healthcare AI
In the next decade, AI systems could vastly improve coordination among care providers, reducing redundant procedures and unnecessary hospitalizations. By identifying high-risk patients early, AI can recommend targeted interventions, potentially avoiding costly emergency treatments. Furthermore, AI-assisted decision-making in chronic disease management can help prevent expensive complications, improving health outcomes while containing costs.
Ethical Concerns for AI in American Healthcare
Nevertheless, successful AI implementation in U.S. healthcare depends heavily on equitable policy and regulatory oversight. Without deliberate intervention, AI technologies may exacerbate existing disparities by disproportionately benefiting affluent regions or institutions. To ensure equitable AI benefits, policymakers must establish clear regulations, encourage transparency, and actively support healthcare organizations serving disadvantaged populations. Consequently, thoughtful AI deployment can transform U.S. healthcare, offering affordable, high-quality care accessible to all Americans.
Practical Steps to Guide AI Towards Positive Outcomes
Regulations for Responsible AI in Healthcare
To ensure AI positively shapes healthcare, establishing robust regulations and ethical guidelines is essential. Currently, rapid AI developments often outpace regulations, leaving ethical questions unanswered. Healthcare policymakers and professional organizations should collaborate to create comprehensive frameworks, clearly addressing accountability, patient privacy, transparency, and fairness. For example, clear guidelines on algorithm transparency and validation standards could prevent biases and enhance patient trust. Consistent oversight will also be necessary, regularly assessing AI systems’ effectiveness and ethical compliance.
Investing in Education for Healthcare AI Literacy
Healthcare professionals must receive proper training to effectively integrate AI into their daily practice. Currently, gaps in AI literacy among clinicians limit successful adoption. Educational programs should focus on teaching healthcare providers how to interpret AI outputs, identify potential biases, and communicate AI-driven recommendations clearly to patients. Similarly, patients should receive education on AI use in healthcare, improving their understanding, comfort, and trust in these advanced technologies.
Promoting Equitable Access to AI Healthcare
Equity should be central to AI integration strategies in healthcare. Without deliberate action, AI-driven solutions risk widening existing health disparities. Therefore, healthcare organizations, policymakers, and technology developers must actively invest in providing equal access to AI-driven healthcare across diverse communities. Supporting underserved areas with affordable AI tools, training, and infrastructure can significantly reduce inequalities, ensuring everyone benefits from technological advancements in healthcare.
Conclusion: Ensuring a Positive Future for AI in Healthcare
Artificial intelligence in healthcare and medicine holds immense potential to dramatically improve patient care, outcomes, and lifespan. Over the next 10-50 years, AI-driven innovations in diagnostics, personalized treatments, surgery, drug discovery, mental health support, longevity research, and public health promise transformative benefits. However, achieving these benefits requires actively addressing significant ethical, social, and practical challenges.
To fully realize AI’s potential, healthcare providers, policymakers, and society as a whole must prioritize ethical and equitable implementation. Transparency, accountability, robust regulations, and equitable access will help build public trust and ensure technologies benefit everyone—not just privileged populations. Furthermore, ongoing education for both healthcare providers and patients can ensure AI integration enhances, rather than replaces, compassionate human care.
Ultimately, the success of AI in healthcare depends heavily on thoughtful human oversight and careful management of potential risks. By proactively addressing privacy concerns, algorithmic bias, healthcare inequalities, and automation ethics, we can steer AI technology in healthcare toward a future that genuinely benefits human health. The promise of artificial intelligence is not inevitable—it depends entirely on choices we make today. With responsible guidance and deliberate action, AI has the potential to create a healthier, more equitable, and hopeful future for healthcare globally.
Also consider how AI could affect human jobs.
Sources:
- World Economic Forum. (2023). AI in Healthcare: Revolutionizing Diagnostics and Patient Care. Retrieved from Visit External Link
- Stanford University Human-Centered Artificial Intelligence. (2024). Ethical Challenges of AI in Healthcare. Retrieved fromVisit External Link
- Centers for Disease Control and Prevention (CDC). (2023). AI in Public Health Surveillance and Prevention. Retrieved fromVisit External Link
- National Institutes of Health (NIH). (2024). Artificial Intelligence and Personalized Medicine. Retrieved fromVisit External Link
- Harvard Medical School. (2023). AI and Robotics in Surgery: Opportunities and Risks. Retrieved fromVisit External Link
- The Lancet Digital Health. (2024). Artificial Intelligence in Mental Health Care: Balancing Innovation and Ethics. Retrieved from Visit External Link
- Organisation for Economic Co-operation and Development (OECD). (2024). Healthcare Access Inequality and AI. Retrieved from Visit External Link
- MIT Technology Review. (2023). Drug Discovery and Biotechnology Advances Powered by AI. Retrieved from Visit External Link
- McKinsey & Company. (2024). Longevity Science and AI: Extending Human Healthspan. Retrieved from Visit External Link
- Johns Hopkins University. (2023). AI in Healthcare: Improving Efficiency or Deepening Inequality? Retrieved from Visit External Link